For most people, chronic pelvic pain starts as a dull ache or a sudden sharp sensation that worsens with activities like exercising, moving around, or even sitting at a desk. It’s not just a minor discomfort; it can make everyday tasks feel difficult and draining. What can be done to address this pain?
So this blog will give you the answer you need. It highlights the causes and symptoms of chronic pelvic pain, including how it can overlap with other conditions. By understanding these signs, you can take the first step towards effective treatment and better management of your pelvic health.
What is Chronic Pelvic Pain?
Chronic Pelvic Pain (CPP) refers to persistent lower abdominal or pelvic pain lasting for six months or more. It’s more than just a passing ache or cramps. Chronic pelvic pain can disrupt your daily activities, making it hard to live a normal life.
Symptoms:
- Persistent pain in the lower abdomen, pelvic region, or lower back.
- Associated symptoms include fatigue, depression, and anxiety.
What does “Pelvic Pain Lasting More Than Six Months” mean?
When pelvic pain persists beyond the typical duration of menstrual cycles or post-injury recovery, it’s considered chronic. This type of pain can vary in intensity, from dull aches to sharp, stabbing sensations. The discomfort can be constant or intermittent, but the long duration makes it harder to ignore.
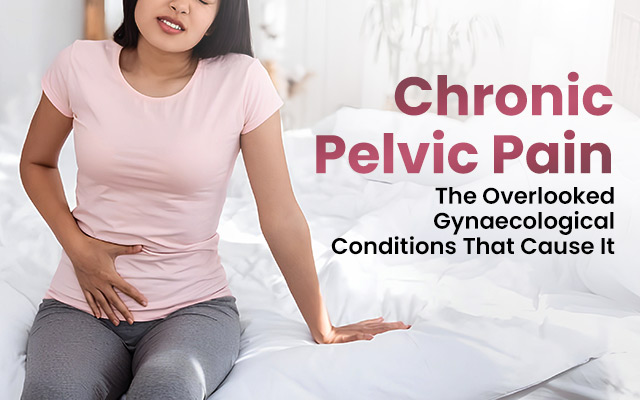
Common Gynaecological Causes of Chronic Pelvic Pain
Several underlying gynaecological conditions are commonly associated with chronic pelvic pain. Identifying these causes is crucial for managing the condition and seeking appropriate treatment. Let’s take a closer look at some of the most common conditions.
Now, as you have the information, let’s know everything in detail
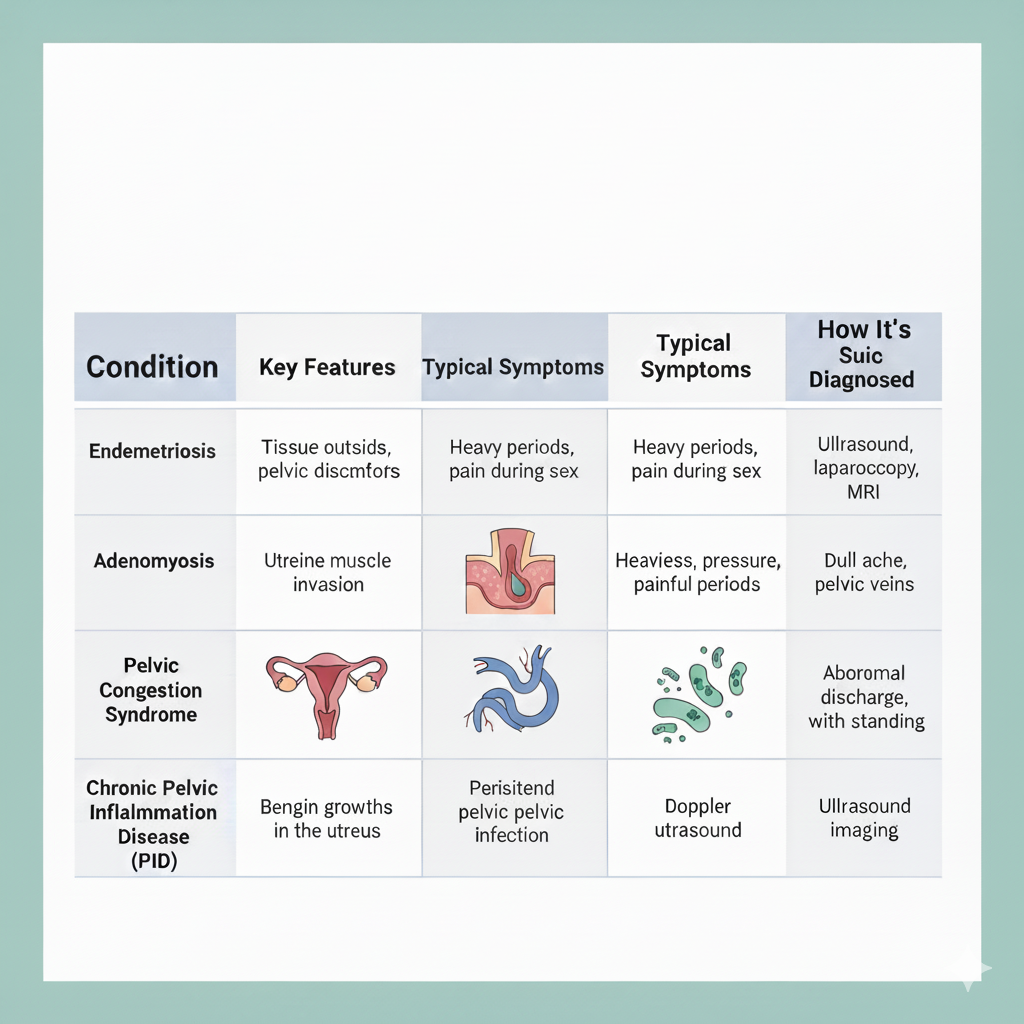
Endometriosis
Endometriosis is one of the leading causes of chronic pelvic pain. It occurs when tissue similar to the uterine lining grows outside the uterus, leading to inflammation, scarring, and intense pain. This pain often worsens during retrograde menstruation, which happens when menstrual blood flows backwards into the pelvic cavity instead of leaving the body.
Did you know?
Endometriosis affects an estimated 10% (190 million) of reproductive-age women worldwide. (Source)
Adenomyosis and Painful Uterine Heavy Periods
Adenomyosis occurs when endometrial tissue grows into the muscular walls of the uterus.
Symptoms:
- Causes heavy periods
- Leads to severe cramps
- Results in pain during intercourse
Additional Symptoms: Often accompanied by excessive bleeding.
Fibroids
Fibroids are non-cancerous growths that develop in the uterus. While many fibroids don’t cause symptoms, those that do can lead to chronic pelvic pain. The pressure exerted by large fibroids on nearby organs can cause discomfort during movement, sexual activity, or even regular sitting.
Symptoms:
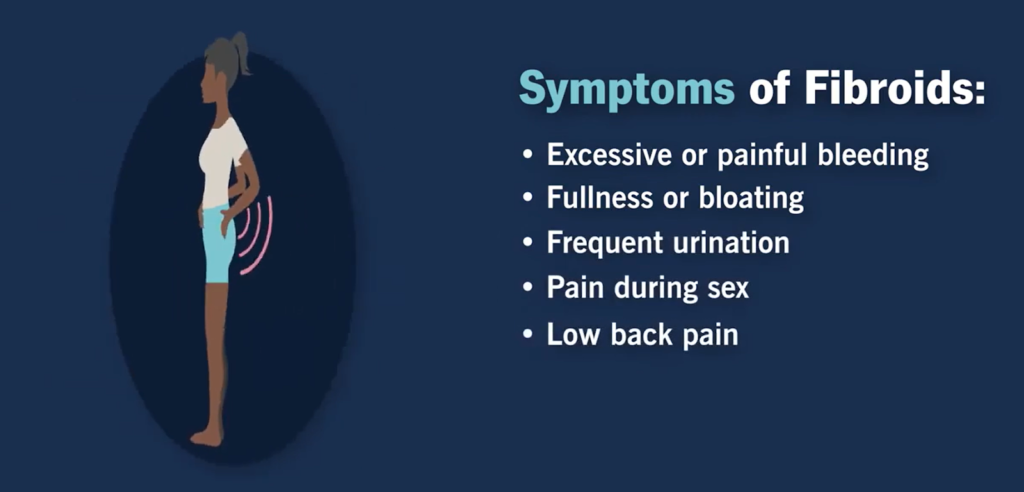
- Excessive or painful bleeding
- Fullness or bloating
- Frequent urination
- Pain during sex
- Low back pain
Pelvic Congestion Syndrome
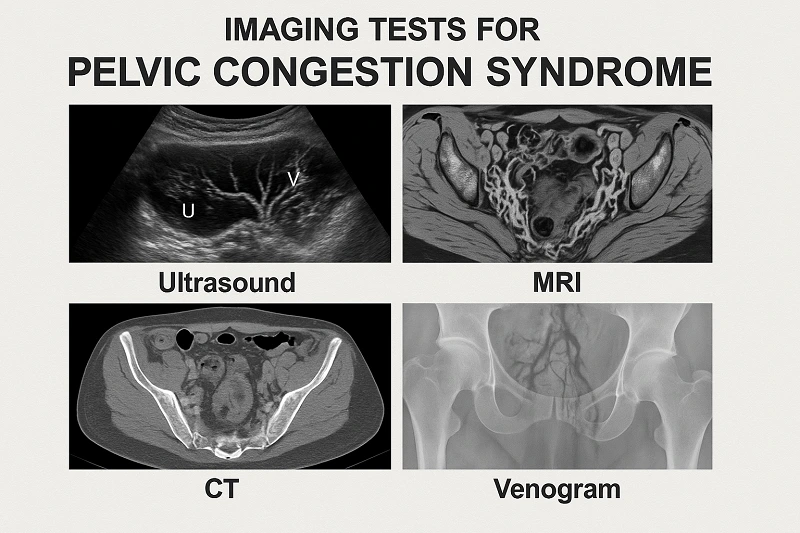
Pelvic congestion syndrome occurs when veins in the pelvis become enlarged and varicose. This can lead to a feeling of fullness or heaviness in the pelvic area, resulting in constant pelvic discomfort. The pain typically worsens with standing or physical activity.
The imaging test to treat pelvic congestion syndrome:
- Ultrasound
- MRI
- CT
- Venogram (invasive procedure)
Chronic Pelvic Inflammatory Disease (PID) & Complications
Pelvic inflammatory disease is an infection of the reproductive organs, often caused by untreated sexually transmitted infections (STIs). If left untreated, PID can lead to scarring, blocked fallopian tubes, and chronic pelvic pain, all of which can make it difficult for women to conceive.
Hidden Causes of Chronic Pelvic Discomfort
Chronic pelvic pain isn’t always purely gynaecological in nature. It can overlap with other health conditions, such as digestive disorders, urinary tract issues, and musculoskeletal concerns. These overlapping conditions often complicate diagnosis and make treatment more challenging.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a common digestive condition that can cause abdominal pain, bloating, and discomfort. These symptoms can overlap with chronic pelvic pain, making it harder to pinpoint the exact cause of the discomfort. Women with IBS often experience chronic pelvic pain, especially if they also suffer from endometriosis or fibroids.
Bladder Conditions & Painful Bladder Syndrome
Painful bladder syndrome, also known as interstitial cystitis, causes pelvic pain associated with bladder inflammation. This can be mistaken for gynaecological issues, as the pain often feels similar to that of pelvic infections or fibroids. If bladder conditions go untreated, they can exacerbate pelvic pain and discomfort.
Musculoskeletal Issues and Pelvic Floor Dysfunction
Pelvic floor dysfunction occurs when the muscles of the pelvic region don’t function properly. This can cause pain during movement, bowel movements, or sexual activity. Additionally, musculoskeletal issues like hip problems or lower back pain can often contribute to or cause pelvic discomfort.
Because pelvic pain often overlaps with digestive, bladder, and muscle-related issues, consulting Dr. Smita Jadhav, an experienced gynecology doctor in Salt Lake, ensures an accurate diagnosis and the right treatment approach.
Symptoms of Chronic Pelvic Pain
Recognising the signs of chronic pelvic pain is the first step toward treatment. The symptoms can vary, but the pain is typically persistent and worsens with certain activities, such as sex, exercise, or menstruation.
| Symptoms | Description |
| Pain That Doesn’t Go Away | Chronic pelvic pain lasts for months or years, varying in intensity. It doesn’t subside after a few days or weeks. |
| Changes in the Menstrual Cycle | Many women experience heavy bleeding, irregular periods, or abnormal cycles, often linked to conditions like endometriosis or fibroids. |
| Pain During Sex | Pain during intercourse is common, especially with endometriosis or pelvic floor dysfunction, affecting quality of life. |
Tests and Procedures to Diagnose Chronic Pelvic Pain
- Pelvic Ultrasound: Useful for detecting fibroids, ovarian cysts, and other abnormalities.
- Laparoscopy: A minimally invasive surgical procedure that allows doctors to visually examine the pelvic organs for conditions like endometriosis.
- MRI: Provides detailed images of the reproductive organs, helping to identify issues such as adenomyosis.
Treatments and Management
Managing chronic pelvic pain requires a comprehensive approach that addresses both the underlying condition and the symptoms. Treatment options may include medication, lifestyle changes, or even surgery.
Pain Relief Medications
Over-the-counter pain relievers can help manage mild pain. In some cases, stronger prescription medications, including hormonal treatments, may be needed to control pain associated with conditions like endometriosis.
Hormonal Therapy and Surgery
For conditions such as endometriosis, hormonal therapy may be used to suppress tissue growth. Surgery, such as laparoscopy, can also be effective in removing adhesions or endometrial growths.
Physical Therapy for Pelvic Floor Dysfunction
Pelvic floor therapy can be incredibly effective in managing pain caused by pelvic floor dysfunction. It helps strengthen the muscles and improve overall pelvic health.
Finding Relief from Chronic Pelvic Pain
Chronic pelvic pain can stem from various underlying conditions, making it crucial to identify the exact cause for effective treatment. From gynaecological issues like endometriosis and fibroids to digestive and musculoskeletal factors, understanding these triggers can help manage and alleviate discomfort.
If you’re experiencing persistent pelvic pain, it’s important to consult with a specialist to find the right solution. Consult Dr. Smita Jadhav, an experienced gynecology doctor in Salt Lake, to get personalised care and a clear diagnosis for your pelvic pain. Book your appointment today.
For more information, call +91 9748825624
People Also Ask (FAQs)
1. What exactly is chronic pelvic pain?
Chronic pelvic pain is defined as pain that lasts for six months or more, affecting the lower abdomen or pelvic area.
2. Can chronic pelvic pain be a sign of endometriosis?
Yes, endometriosis is one of the most common causes of chronic pelvic pain and often worsens during menstruation.
3. Do fibroids cause chronic pelvic pain?
Fibroids can cause discomfort due to the pressure they place on pelvic organs, leading to cramping and painful periods.4. Why do some women have chronic pelvic pain even with normal tests?
In some cases, pain is due to pelvic floor dysfunction, IBS, or bladder conditions, which may not always show up on standard tests.