You’ve been living with discomfort from fibroids or endometriosis, you’re worried about a major surgery, long hospital stay, big scar, and then your doctor offers you an alternative: a procedure with tiny incisions, less pain, shorter rest time, and you’re back to your life sooner. That’s precisely what minimally invasive gynaecological procedures can do.
If you’re looking for a gynaecology doctor in Saltlake, Kolkata, this blog is for you. Let’s walk through what these procedures are, why they matter, and how they might change your healing experience for the better.
What Are Minimally Invasive Gynaecological Procedures?
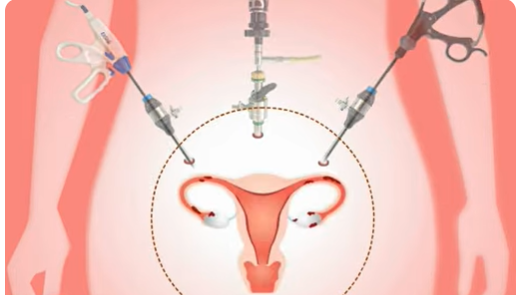
Simply, instead of a large “open” cut across the abdomen, minimally invasive techniques use small incisions (sometimes one), tiny cameras and specialised instruments to treat gynaecological conditions. These include:
- Laparoscopic Gynaecological Procedures – small abdominal cuts, camera inside the belly.
- Hysteroscopic Surgery – access through the vagina/cervix to treat inside the uterus (no big cut).
- Minimally Invasive Hysterectomy – removal of the uterus by minimal access rather than a whole open abdomen.
Compared with traditional “open” surgery, these options aim to reduce trauma, shorten recovery, and look more cosmetically appealing.
Types of Minimally Invasive Gynaecological Procedures
Let’s peek under the hood—what are the actual techniques?
Laparoscopic Surgery
In this method, the surgeon makes small incisions in the abdomen, inserts a camera (laparoscope), and operates with instruments. It’s widely used and has strong evidence of benefit.
Hysteroscopic Surgery
Access is through the vagina and cervix into the uterus (no abdominal incision). This is ideal for inside-uterus problems.
Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES)
A newer method where surgical access is through natural orifices (like the vagina). Minimises visible scars even further.
Minimally Invasive Hysterectomy
This may combine laparoscopic, robotic or vaginal approaches rather than full open abdomen. Minimised recovery, less trauma.
Benefits of Minimally Invasive Techniques
What’s really in it for you? Here are key benefits with examples and a simple table to help cleanly compare.
Faster Recovery Time
Since the access is less invasive, the body has less trauma to heal. Studies show that patients often leave the hospital earlier and return to daily life more quickly.
Reduced Pain and Blood Loss
Fewer incisions = less skin and muscle damage = less pain and bleeding. For instance, laparoscopic and robotic surgeries have been shown to reduce intraoperative blood loss compared to open surgery.
Smaller Incisions and Minimal Scarring
Tiny cuts usually mean more minor, less noticeable scars—and often a better cosmetic outcome. For many patients, this is a meaningful bonus.
Shorter Hospital Stays
Because recovery is faster and complications are fewer, you may go home earlier—or even the same day (in outpatient surgery).
Lower Risk of Infection
Less exposure, more minor wounds, less overall trauma = lower infection risk. There’s evidence that minimally invasive methods reduce postoperative complications.
| Benefit | Traditional Open Surgery | Minimally Invasive Surgery |
| Incision size | Large incision | Small incisions or natural orifice access |
| Recovery time | Longer (weeks) | Shorter (days to a week) |
| Pain & blood loss | More likely | Less likely |
| Hospital stay | Longer | Shorter or outpatient |
| Scarring | Larger scar | Minimal scar |
| Infection risk | Higher | Lower |
Common Conditions Treated with Minimally Invasive Surgery
Let’s see where these techniques shine—what kinds of issues can they handle? If you’re visiting Dr Smita Jadhav, a trusted gynaecologist in Saltlake, you’ll want to know your options.
- Uterine Fibroids: Non-cancerous growths in the uterus. The technique known as “fibroid removal minimally invasive fibroid removal” (sometimes laparoscopic myomectomy) allows removal with minimal access.
- Endometriosis: Tissue outside the uterus causing pain or infertility. “Endometriosis laparoscopic treatment” is commonly used to excise or ablate affected tissue.
- Pelvic Organ Prolapse: When organs like the bladder or uterus descend. “Pelvic organ prolapse surgery” can be done minimally invasively in many cases.
- Ovarian Cysts: Fluid-filled sacs on the ovary—many removed via laparoscopy.
- Abnormal Uterine Bleeding: When heavy or irregular bleeding requires intervention, hysteroscopic surgery benefits (inside the uterus) are relevant.
- Endometrial Cancer (in selected cases): Minimally invasive hysterectomy can be used—but note, not all cases are ideal.
Who Is a Candidate for Minimally Invasive Surgery?
Not everyone qualifies—but many do. Your suitability depends on:
- Your general health, fitness level and co-existing conditions.
- The specific condition being treated (size and nature of fibroid, stage of endometriosis, prolapse severity, etc).
- Whether there are complicating factors (previous surgeries, obesity, scar tissue).
- The experience and tools available at your surgical centre and surgeon.
What is the Usual Recovery Timeline
| Time After Surgery | What You Might Be Doing |
| Day 0-1 | Rest, minimal movement, walking in room |
| Week 1 | Short walks, light chores, less pain |
| Weeks 2-4 | Return to most daily tasks, doctor check-up |
| Month 2+ | Full activity (exercise, driving, etc.) |
The Future of Gynaecological Surgery
To wrap it up: if you’re consulting a skilled gynaecology doctor in Saltlake, ask about the minimally invasive options. Procedures like “minimally invasive fibroid removal”, “ laparoscopic endometriosis treatment”, and more are not just fancy labels—they translate into shorter hospital stay, less pain, faster recovery and fewer visible scars. The future is moving firmly in this direction.
That said, surgery is a serious matter, and the choice of open vs minimally invasive depends on many factors. It’s not “one size fits all”. At clinics like Dr Smita Jadhav’s, you will find personalised evaluation and discussion of your unique case.
In short, minimally invasive gynaecological procedures are a true game-changer if you’re looking for better results and a quicker return to life. If you’re thinking about it—or you’ve been told you need a procedure—ask, dig deeper, research, and choose a surgeon and centre experienced in these methods. Your body will thank you.
People Also Ask
What is the difference between open surgery and minimally invasive gynecologic surgery?
Open surgery uses a large incision to access organs; minimally invasive surgery uses small incisions or natural orifices, cameras and specialised tools, leading to less trauma, quicker healing, less pain and shorter hospital stay.
Can all gynaecological conditions be treated with minimally invasive techniques?
No — many can, but not all. Suitability depends on the condition (size, location, complexity), the patient’s health, previous surgeries, and the surgeon’s expertise. For benign conditions like fibroids and endometriosis, many cases qualify; for some cancers or very large/prolapsed organs, open surgery might still be recommended.
How long is the recovery time after minimally invasive gynecologic surgery?
It varies by procedure, but often significantly shorter than open surgery—some patients go home the same day or within 24-48 hours, return to daily activities in 1-4 weeks rather than months.
Are robotic-assisted gynecologic surgeries better than laparoscopic ones?
“Better” depends on many factors. Robotic-assisted surgery offers increased precision and may be helpful in complex cases. But laparoscopic surgery is still excellent and widely used. The surgeon’s skill and case type matter more than the brand of equipment.
Are there any risks specific to minimally invasive gynecologic surgery?
Yes. While overall risks are lower, you still face the usual surgical risks (bleeding, infection, organ injury) and risks specific to the method (need to convert to open surgery, limitations due to access). It’s important to talk through these with your surgeon.